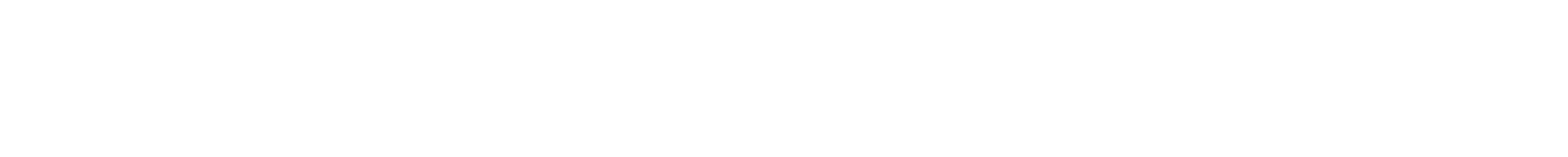
MONTREAL — The Pavillon Camille-Lefebvre long-term care home in southwest Montreal houses some of the patients most vulnerable to succumbing to a pandemic, including 18 who live on ventilators full time.
But as COVID-19 swept through Montreal’s nursing homes like a seemingly unstoppable force, the Pavillon Camille-Lefebvre achieved a rare feat: not a single positive case, much less any COVID-19 deaths.
Montreal is the Canadian hotspot for COVID-19, with over 28,772 cases and 3,437 deaths as of Friday. Around 80 per cent of the province’s deaths have occurred in seniors residences and long-term care homes.
Information obtained from Montreal’s five health boards suggest only a handful of facilities were able to avoid infection. In addition to Pavillon Camille-Lefebvre, those include two private facilities in the northern region, one small facility located within a hospital and one larger public care home.
A few others, including the Montreal Chinese Hospital, were able to stop the virus from spreading despite one or two cases.
Judith Morlese, a nurse-manager at the Pavillon Camille-Lefebvre, believes the facility’s success in keeping out COVID-19 was about more than just luck.
She says rapid action, dedicated infection-control teams and constant communication with staff were some of the keys to keeping the virus at bay, and they could provide a blueprint for other homes to follow if a second wave occurs.
Morlese said acting early, often ahead of the provincial government directives, was central to preventing infection.
The centre began developing a pandemic plan in January, before the first case in the province was declared, and made the decision early on to ban visitors and require staff members returning from overseas to stay home until testing showed they were not infected.
By February, meetings to discuss the pandemic were held daily.
Staff members were brought on board early and subjected to a thorough screening process every day before work. They were told to stay home and get tested at the first appearance of symptoms.
As cases began to crop up elsewhere, anxiety rose. Employees were met at the beginning of every shift and reminded to treat all patients, and each other, as if they were positive.
“We were nervous because we saw what was happening, and we felt bad for our partners in the network, we were scared,” Morlese said in an interview. “So that’s the truth. We were really, really scared.”
Morlese says much of the home’s success came from diligently following the simple health directives regarding sanitizing equipment, hand-washing and wearing of protective equipment.
However, the facility also had two advantages that many of the others didn’t: namely, a skilled infection-control team and the ability to limit staff from working in multiple facilities.
The 135-bed facility is also linked to the Lachine Hospital and is part of the McGill University Health Centre, which proved an advantage because it meant better access to epidemiologists and other experts, according to Morlese.
France Nadon, an infection-control consultant at the home, said part-time workers with multiple jobs were asked not to work elsewhere if they wanted to keep working at the Pavillon.
Those who stayed were offered full-time work, which helped the home to avoid the staff shortages that authorities have cited as a weak point that allowed COVID-19 to enter in so many homes.
Infection-control specialists were on hand to answer employee questions and give refresher courses on the proper use of protective equipment, Nadon said.
Between 10 and 15 employees acquired COVID-19 outside of work, but none of them passed it on to patients — which Nadon says is a tribute to the vigilance they showed when it came to handwashing, disinfecting, and physical distancing.
“They respected the rules, they kept their masks on, they washed their hands and visors,” she said.
Henry Siu, a McMaster University associate professor who has studied long-term care preparedness, says researchers are still studying what factors translate into success in fighting the virus.
While much is unknown, he says the homes that were early adopters of measures such as stricter visitation policies and limiting workers to one facility may have had better outcomes.
In Ontario, he said, private homes seem to have fared worse, possibly because of aging buildings designed to house multiple residents in one room and inadequate space for distancing.
He said that while “luck probably does have a part to play” in which homes suffer major outbreaks, those that are proactive, have up-to-date infection-control protocols and strong leadership “are going to be much better equipped to deal with outbreaks.”
As health authorities warn of a potential second wave, Siu said he’s hopeful that Canadian long-term care homes will be better prepared.
But while they may have become more vigilant about distancing, hygiene and monitoring for symptoms, he said systemic issues, including poor home designs and low pay and poor working conditions that force workers to hold multiple jobs, are harder to solve.
Nadon and Morlese say aren’t celebrating their home’s success just yet.
Though they’re tired, they remain focused on the possibility of a second wave, which could come just as they also have to fight an onslaught of flu and other seasonal respiratory viruses.
Morlese says that while the worry isn’t gone, they feel more prepared this time.
“We’re less stressed because we know what we have to deal with,” she said.
This report by The Canadian Press was first published Aug. 2, 2020
Morgan Lowrie, The Canadian Press