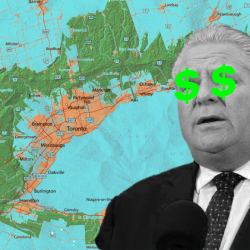
Long-term care homes were neglected as Ontario focused on preparing its hospitals for a potential surge in COVID-19 patients when the pandemic hit, doctors told an independent inquiry recently.
But those nursing homes — which had insufficient personal protective equipment, a lack of universal masking policies and physicians refusing to enter facilities over fears of the virus — were in fact where the surge materialized during the first wave, the Long-Term Care COVID-19 Commission heard.
Doctors from the non-profit Ontario Long-Term Care Clinicians organization testified before the inquiry at the end of September and detailed how ill-prepared the sector was for the spread of the novel coronavirus. The inquiry isn’t open to the public but transcripts of testimony are posted online days later.
“In the first wave we didn’t understand that the surge was happening in long-term care,” said Dr. Evelyn Williams, a longtime physician and past president of the organization.
“There were empty beds in the hospital, and in the long-term care home, which was full, they couldn’t — they didn’t have PPE. They could not actually look after everyone who was sick well because they didn’t have the staff, and they couldn’t move people around.”
COVID-19 tore through long-term care homes in the pandemic’s first wave and has killed more than 1,950 residents. Provincial data shows outbreaks have been increasing in the homes once more as the second wave takes hold.
The commission, led by the Superior Court’s associate chief justice Frank Marrocco, will investigate how the virus spread in the long-term care system and come up with recommendations.
Dr. Rhonda Collins, the chief medical officer of Revera, which owns numerous long-term care facilities in Ontario and across North America, told the inquiry that many homes were directed to keep residents out of hospitals as much as possible in order to free up space in hospitals.
That proved to be a deadly decision after dozens of homes were overwhelmed by the virus, the inquiry heard.
The doctors told the commission that long-term care homes initially followed the World Health Organization’s early guidelines on the novel coronavirus and looked for fever, cough and shortness of breath as symptoms.
“We were unaware at the beginning of this pandemic about asymptomatic spread until after universal masking was recommended in our sector — and it was only recommended after,” said Collins,
“It had already been implemented in the acute care sector. Staff, as well, were only tested if they were symptomatic. Well, many of them were asymptomatic, had not been tested, and were not privy to universal masking strategies.”
It turns out, in hindsight, that the homes were looking for the wrong symptoms, she said.
“What we came to discover is that, especially in our population, atypical symptoms consist of things like delirium, fatigue, anorexia and, in our staff, headaches, muscle aches, fatigue, and things like loss of taste and smell, things that we weren’t expecting for and certainly weren’t looking for,” Collins said.
Long-term care homes also had to deal with some doctors refusing to enter the facilities, while other homes shut out physicians due to lack of personal protective equipment and fear of spreading the virus, Collins said.
The homes had insufficient personal protective equipment because it was being redirected to hospitals, the inquiry heard.
There was also a paucity of direction from various medical bodies to the long-term care sector, the inquiry heard.
While the College of Physicians and Surgeons of Ontario and the Ontario Medical Association provided guidance to family doctors, none was given to long-term care physicians, Collins said.
Problematic staffing levels in the homes, an issue before the novel coronavirus hit, were exacerbated by the pandemic, she said.
Dr. Fred Mather, the organization’s president and the medical director of Sunnyside Home in Kitchener, Ont., said his facility had success after an outbreak in April by transferring patients to hospitals, which were operating at 60 per cent capacity in the area.
“So they had beds,” he said. “And the one facility where I work, we decanted about 60 residents to four local hospitals, and the capacity was there. Some of it, I think, was a bit too late, but once we co-ordinated our efforts, it did work well.”
Marrocco asked what the doctors would suggest long-term care homes do should hospitals be overrun in the second wave but long-term care residents need to be moved.
Mather said there is some capacity in so-called “blessed units” that are used for short-term stays that are relatively empty due to the pandemic, but Collins said more co-ordination is needed quickly to figure out options for the sector.
This report by The Canadian Press was first published Oct. 12, 2020.
Liam Casey, The Canadian Press